Guide to a Low FODMAP Diet for IBS Management
Implementing a Low-FODMAP Diet
Successful adoption requires meticulous preparation and professional guidance. Registered dietitians specializing in digestive health can create customized meal plans that meet nutritional requirements while avoiding high-FODMAP ingredients. Many patients benefit from using food tracking apps specifically designed for FODMAP monitoring, which simplify the identification of problematic foods.
Grocery shopping demands increased vigilance, as many processed foods contain hidden FODMAP sources like onion powder or high-fructose corn syrup. Learning to decipher ingredient lists and recognizing alternative names for problematic compounds becomes second nature with practice. Meal prepping with approved ingredients helps maintain dietary compliance during busy weeks.
Long-Term Management and Considerations
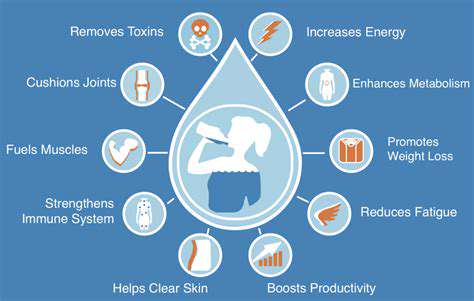
While the low-FODMAP approach provides relief for many, it represents just one component of comprehensive IBS management. Stress reduction techniques, regular physical activity, and adequate sleep all contribute to gut health. Some patients find complementary therapies like cognitive behavioral therapy or gut-directed hypnotherapy enhance their symptom control.
Nutritional monitoring remains crucial, as long-term restriction of certain food groups may impact micronutrient intake. Periodic reassessment with healthcare providers ensures the dietary approach continues to meet both digestive and overall health needs. Many patients ultimately develop an individualized eating pattern that balances symptom control with dietary enjoyment.
Environmental factors frequently influence migraine occurrence. Recognizing personal triggers enables proactive management strategies. Maintaining a detailed symptom diary often reveals unexpected patterns and preventable triggers.
Managing IBS with a Low-FODMAP Diet: Beyond the Food Choices
Understanding the Low-FODMAP Diet for IBS
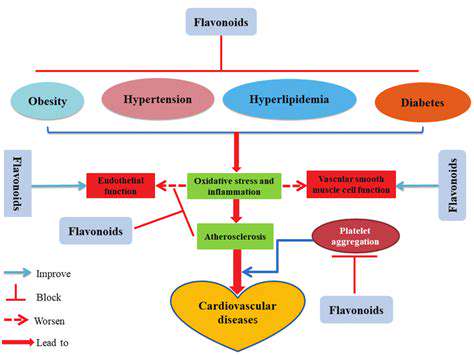
This scientifically validated dietary intervention operates on the principle of reducing osmotic activity and fermentation in the gut. Unlike generic healthy eating guidelines, the low-FODMAP protocol specifically targets carbohydrates that exert excessive osmotic pressure or undergo rapid bacterial fermentation. The diet's effectiveness stems from its precision in addressing the underlying mechanisms of IBS symptoms rather than simply avoiding irritating foods.
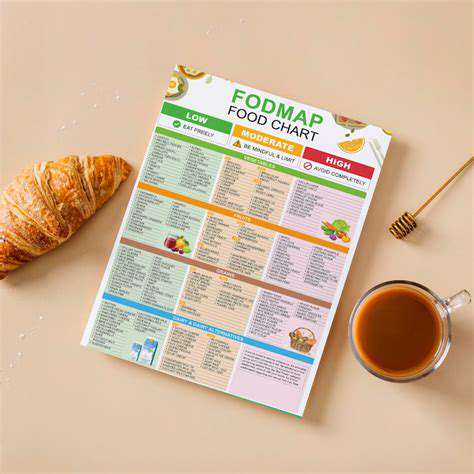
Identifying FODMAP-Rich Foods
FODMAP content varies significantly based on multiple factors. For instance, the ripeness of bananas dramatically affects their fructose content - green bananas contain resistant starch (a FODMAP) while ripe bananas contain more simple sugars. Similarly, cooking methods can alter FODMAP levels; roasting onions concentrates their fructans while boiling may leach some into the cooking water. These nuances underscore the importance of professional guidance when navigating the diet's complexities.
Practical Strategies for Meal Planning
Effective implementation involves creative ingredient substitutions. Swap onion and garlic for infused oils that provide flavor without the fructans. Replace wheat pasta with gluten-free alternatives made from rice or corn. Many patients develop personalized safe food lists that include versatile low-FODMAP staples like quinoa, carrots, and firm tofu. Batch cooking and freezing individual portions helps maintain dietary consistency during busy periods.
Navigating Social Situations and Restaurants
Dining out requires proactive communication and strategic menu selections. Ethnic cuisines like Japanese or Thai often feature naturally low-FODMAP options when modified appropriately. Calling ahead to discuss dietary needs with restaurant staff increases the likelihood of successful meals. When attending social gatherings, bringing a dish to share ensures at least one safe option while educating others about dietary needs.
Long-Term Management and Sustainability
The ultimate goal involves establishing a personalized, flexible eating pattern that maximizes food variety while minimizing symptoms. Many patients progress to a modified low-FODMAP approach after completing the reintroduction phase, maintaining restrictions only on their identified triggers. Regular follow-ups with a dietitian help adjust the diet as tolerance levels change over time. This adaptive approach promotes both physical comfort and psychological well-being.







![Seasonal Ingredient Guide for Winter [2025]](/static/images/28/2025-06/CitrusFruits3AABurstofWinterSunshine.jpg)